Hot from the press: A new study from 2023!
I am thrilled to share the newest study by Dr. Aristo Vojdani (Vojdani et al., 2023), one of my all-time favorite researchers and humans.
The study addresses details behind “viral persistence” in Long COVID and acknowledges EBV as one of the factors that “may contribute to inflammation and autoimmunity in long COVID”. The most common long COVID symptoms the study lists are:
- fatigue,
- brain fog,
- difficulty sleeping,
- arthralgia [pain in the joint],
- myalgia,
- pharyngitis,
- fever,
- headaches,
- gastrointestinal symptoms,
- skin rashes,
- and affective symptoms including depression and anxiety.
Incidentally, this entire list is exactly what common EBV presentations are. To.The. Dot.
Reactivation of latent viruses such as EBV and human herpes virus 6 (both associated with pathology of myalgic encephalomyelitis and chronic fatigue syndrome) in long COVID has been associated with the severity and length of COVID 19 symptoms. According to the study, EBV reactivation “facilitates the entry of the SARS-COV-2 into cells, enhancing viral load and severity of symptoms”. Dr. Viojdani maps out the specific detailed mechanisms of how this process happens (for those of you into science).
Most importantly, the study proposes testing for EBV (herpes 6 and CMV) in long COVID cases.
Long haul COVID, COVID and EBV coinfections, and post-vaccination EBV reactivations are all common topics of concern in the EBV community. My goal for this blog is to bring in the research we have available and put the studies in the context of what I observe in our community.
Before we address medical literature,
I can confirm that it is common for COVID to make EBV worse
– we do get a lot of complaints about that, which we will explain further.
Research on COVID and EBV
We have just a few studies so far and more are needed, but we can definitely make very good conclusions based on the research available. Interestingly, some smart researchers started to test both EBV and COVID earlier during the COVID pandemic in those hospitalized with COVID, even in the Wuhan hospital.
We do know from research that
there may be a higher incidence of EBV in people with COVID.
That there are links between long-haulers with COVID and EBV reactivation, which we still do not understand fully. Which one triggers the other?
How does COVID-19 affect you if you have EBV?
Anecdotal evidence:
Here is what we see in the EBV community (in research this is called “anecdotal evidence”) – this is feedback I get from people that reach out to me and from our students and clients, not from medical studies. In short, this is not statistically validated or shown in studies. This is just a pattern I have observed and most likely has a subjective bias based on the community I serve.
While we are still waiting for more studies,
“The consistent feedback I get is that COVID seems to
contribute to often a severe reactivation of EBV in people
who already suffer from chronic active EBV (CAEBV).”

This is consistent with the well-studied concept of “transactivation” – reactivating viruses like EBV as a result of another unrelated acute infection. (White et al., 2006)
COVID-19 and EBV
What about EBV and COVID vaccination? It is a mixed bag, but I would say that
“There is a pattern of severe EBV reactivations post COVID vaccination.”
Again, this is not statistically relevant as this is just my observation and feedback I get. On the flip side, while not common, in just a few cases, the vaccine actually seemed to provide an immune reset for EBV and improved functionality. Some people with EBV do not have any issues post-vaccine. On average, based on the feedback I get, more often than not, people with EBV suffer more EBV reactivations post-vaccine. I will share a study on this further in this blog. In the meantime, let’s take a look at existing studies on COVID and EBV to see what patterns are evident.
COVID-19 and EBV Studies
“Investigation of Long COVID Prevalence and Its Relationship to Epstein-Barr Virus Reactivation” (Gold et al., 2021)
A study from June 2021 suggests that EBV reactivates either at the same time as COVID-19 infection starts or soon after.
“EBV may therefore play a major role in post-COVID fatigue and brain fog
– in many if not most cases!” (Gold et al., 2021)
Which is first, the chicken or the egg?
With the COVID long-haulers, is it EBV or COVID? A study suggests that nearly 73% of COVID “long haulers,” had reactivated EBV at the same time. That is a very substantial percentage of the long haulers population.
Here is a summary:
Jeffrey E. Gold, one of the researchers in the study on long COVID, stated that they ran Epstein-Barr virus serological tests on COVID-19 patients at least 90 days after testing positive for SARS-CoV-2 infection, comparing EBV reactivation rates of those with long COVID symptoms to those who never experienced long COVID symptoms. They found
“[…] over 73% of COVID-19 patients who were experiencing long COVID symptoms
were also positive for EBV reactivation.” (Gold et al., 2021)
While EBV reactivation may not be responsible for all cases of recurring fatigue or brain fog after recovering from COVID-19, evidence indicates that it likely plays a role in many or even most cases. I can confirm this based on what i see in our EBV community.
“Positive Epstein–Barr virus detection in coronavirus disease 2019 (COVID-19) patients” (Chen et al., 2021)
This is a study published in May 2021 from the Wuhan University Hospital and included patients with COVID-19 alone and COVID and EBV at the same time, over a period of 2 months Jan- Feb 2020. This is a prospective study, so it looked at what had already happened to that particular group, based on labs that had been taken at the time. 55.2% of the COVID group also had EBV coinfection, based on (+) VCA IgM antibody.
I thought you would want to see the most common symptoms in the group with both infections and just with COVID. The “Negative” column will be COVID-19 alone:
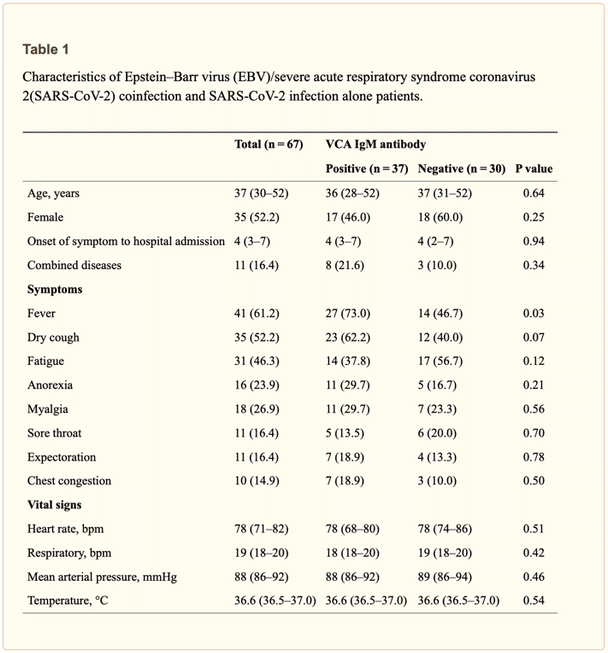
As you can see above, there was more fever and dry cough in the EBV and COVID-10 coinfection group, but otherwise symptoms overlapped: fatigue, myalgia, lack of appetite (anorexia). The co-infection group had 3.09 times (so 300%) risk of developing fever than the COVID group. (Chen et al., 2021)
The researchers provided complete blood test results as well, and to summarize, immune cell function in the coinfection group was in general a tiny bit lower, but not statistically significant, which makes sense as the body had to fight more viruses. One thing of note statistically was that ALT and AST, two liver enzymes, were higher in the coinfection group. Of course, it makes sense too as the liver had to work harder.
You will be happy to hear that there was no statistical significance in the prevalence of patients going to the ICU and that no patients died in that study group.
Here is their conclusion, in their own words:
“(1) more than half of COVID-19 patients were positive for EBV VCA IgM antibody;
(2) EBV VCA IgM antibody was associated with fever, higher CRP and higher AST;
(3) the EBV/SARS-CoV-2 coinfection patients were more likely to be given corticosteroid therapy by doctors;
(4) The CD8 count in EBV/SARS-CoV-2 coinfection patients was a little less than that in SARS-CoV-2 infection alone patients.”

The study concluded that those that had both COVID and EBV were three times more likely to develop a fever, and had more dry cough. So in general, COVID may be a bit more severe. But the risk of ending up in ICU (just because they had EBV along with COVID) was not higher.
“High incidence of Epstein–Barr virus, cytomegalovirus, and human-herpes virus-6 reactivations in critically ill patients with COVID-19” (Simonnet et al, 2021)
This study was based on the premise that “systemic reactivation of herpes viruses may occur in intensive care unit (ICU) patients and is associated with morbidity and mortality”. It was a retrospective study, again, looking at findings that had already been recorded. They analyzed 34 selected patients previously admitted to the ICU for confirmed COVID-19 induced acute respiratory failure, who underwent systematic testing for Epstein–Barr virus (EBV), cytomegalovirus (CMV) and human-herpes virus-6 while in the ICU. They found that 82% had EBV, while only 15% had CMV and 22% had HHV6. That is a huge difference and a very high incidence in EBV.
“Clinical characteristics and outcomes of critically ill patients with acute COVID-19 with Epstein-Barr virus reactivation” (Xie et al., 2021)
This is a study from Sept 2021, again with critical cases from ICU. The conclusion was that those with concurrent EBV and COVID had higher 28-day and 14-day mortality rates and received more immune-supportive treatments than those with COVID but without EBV.
COVID-19 Vaccination and EBV Studies:
We repeatedly get complaints in our EBV community of a severe EBV reactivation post COVID-19 vaccination. While this is anecdotal as we did not conduct a study to actually provide statistics, it is much more prevalent than not having worsening EBV. This is consistent with studies.
“Increased EBV DNAemia after Anti-SARS-CoV-2 Vaccination in Solid Organ Transplants” (Musalik et al., 2022)
This study found that COVID-19 vaccination led to a significant increase in the presence of the virus in the blood and even EBV reactivation. In the group of ten liver and kidney transplant patients, nine had a significant increase in EBV in the blood while a single patient who had previously been negative for EBV for an extended period had an EBV reactivation.

COVID-19 Vaccination and other Herpes Viruses (like shingles) Studies:
Studies have reported varicella zoster (shingles, which is also a herpes virus) and other herpes viruses reactivating post COVID-19 vaccination:
“Varicella-zoster virus reactivation after SARS-CoV-2 BNT162b2 mRNA vaccination: Report of 5 cases” (Rodriguez-Jimenez et al., 2021)
This study included 3007 people (residents and health workers) vaccinated for COVID-19 in an elderly community home in Spain. After the first dose, there were three cases of shingles, and two more were reported after the second dose. Those with shingles were healthy adults (between 39 and 58 years of age, two men and three women), and their blood count did not show any abnormality. Their symptoms varied, from skin lesions, to pain, to fever. This is worth noting since this virus does not typically reactivate following vaccinations. Again, varicella-zoster virus is a herpes virus, like EBV.

“Herpes zoster following inactivated COVID-19 vaccine: A coexistence or coincidence?” (Bostan et al., 2021)
Unfortunately, there is no free access to the full study or even its abstract.
“Reactivation of Herpes Zoster Virus After COVID-19 Vaccination: Is There Any Association?” (Agrawal et al., 2022)
This study reports on ten cases of shingles reactivated 7 to 21 days after the COVID-19 vaccination. Researchers conclude: “transient immunomodulation following vaccination, similar to that seen in COVID-19 illness, could be one explanation for this reactivation.” The study provides photos of severe skin lesions and a table with specific symptoms of each person.
How to Heal from Long Covid or Post-Vaccination EBV Reactivation
First things first, know that you can get better. We do have ample resources for you. Your starting point would be scheduling a Clarity Call and looking over our EBV Recovery Program and EBV Masterclass Series. Both these offerings address in-depth how to recover from EBV Reactivation due to contracting COVID or receiving a COVID vaccination.
Schedule a Clarity Call with Dr. Kines
Learn More about our EBV Recovery Program
Watch the On-Demand EBV Masterclass Series
References:
Agrawal, S., Verma, K., Verma, I., & Gandhi, J. (2022). Reactivation of Herpes Zoster Virus After COVID-19 Vaccination: Is There Any Association? Cureus, 14(5), e25195. doi:10.7759/cureus.25195
Bostan, E., & Yalici-Armagan, B. (2021). Herpes zoster following inactivated COVID-19 vaccine: A coexistence or coincidence? J Cosmet Dermatol, 20(6), 1566-1567. doi:10.1111/jocd.14035
Chen, T., Song, J., Liu, H., Zheng, H., & Chen, C. (2021). Positive Epstein-Barr virus detection in coronavirus disease 2019 (COVID-19) patients. Sci Rep, 11(1), 10902. doi:10.1038/s41598-021-90351-y
Gold, J. E., Okyay, R. A., Licht, W. E., & Hurley, D. J. (2021). Investigation of Long COVID Prevalence and Its Relationship to Epstein-Barr Virus Reactivation. Pathogens, 10(6). doi:10.3390/pathogens10060763
Musialik, J., Kolonko, A., & Wiecek, A. (2022). Increased EBV DNAemia after Anti-SARS-CoV-2 Vaccination in Solid Organ Transplants. Vaccines (Basel), 10(7). doi:10.3390/vaccines10070992
Rodriguez-Jimenez, P., Chicharro, P., Cabrera, L. M., Segui, M., Morales-Caballero, A., Llamas-Velasco, M., & Sanchez-Perez, J. (2021). Varicella-zoster virus reactivation after SARS-CoV-2 BNT162b2 mRNA vaccination: Report of 5 cases. JAAD Case Rep, 12, 58-59. doi:10.1016/j.jdcr.2021.04.014
Simonnet, A., Engelmann, I., Moreau, A. S., Garcia, B., Six, S., El Kalioubie, A., . . . Jourdain, M. (2021). High incidence of Epstein-Barr virus, cytomegalovirus, and human-herpes virus-6 reactivations in critically ill patients with COVID-19. Infect Dis Now, 51(3), 296-299. doi:10.1016/j.idnow.2021.01.005
Vojdani, A., Vojdani, E., Saidara, E., & Maes, M. (2023). Persistent SARS-CoV-2 Infection, EBV, HHV-6 and Other Factors May Contribute to Inflammation and Autoimmunity in Long COVID. Viruses, 15(2). doi:10.3390/v15020400
White, M. K., Gorrill, T. S., & Khalili, K. (2006). Reciprocal transactivation between HIV-1 and other human viruses. Virology, 352(1), 1-13. doi:10.1016/j.virol.2006.04.006
Xie, Y., Cao, S., Dong, H., Lv, H., Teng, X., Zhang, J., . . . Wang, R. (2021). Clinical characteristics and outcomes of critically ill patients with acute COVID-19 with Epstein-Barr virus reactivation. BMC Infect Dis, 21(1), 955. doi:10.1186/s12879-021-06638-y





Leave A Comment