How is EBV Diagnosed?
Diagnosis of EBV is the trickiest part of your EBV journey. And you may already know this if you have been lucky enough to get the right labs done and interpreted, or if you are in the process of trying to figure out what to test or where to find a doctor willing to run the tests for you.
For many, this remains a challenge because, commonly, medical doctors believe that since most of the global population has antibodies to EBV, testing is not practical—a positive result would only indicate past exposure. It also really depends on what exactly you are testing!
If You Need to Test:
Did You Know?
You CAN test for EBV without your doctor today!
You no longer have to knock from door to door trying to find a medical doctor to agree to test your EBV for you. You also no longer need to search which test panel to ask for. We partnered with Ulta Labs, a direct-to-consumer lab, which offers very good prices for over 2000 tests. They offer the panel of all four main antibodies you should test. This lab test is available in the USA except these states: NY, NJ, and RI.

A lot of people that suffer and have a high risk or likelihood of CAEBV spend months or even years trying to get proper testing, and if you are one of those people, I encourage you NOT to wait, but to use this or another direct-to-consumer lab available in your location and get the testing done. Hopefully, the information provided on this website page will help you navigate the main complexities of your lab results, but if you need more help, my book The Epstein Barr Virus Solution has much more information on the many possible testing results scenarios.
Diagnosis in Children
Often a child will have a mild EBV infection that may go unnoticed, e.g., appearing as short-lived mild flu-like symptoms. A more pronounced EBV infection can cause fatigue or weakness, sore muscles, loss of appetite, fever, sore throat with swollen tonsils (possibly with white patches), swollen lymph nodes (in the neck, underarms, and groin), and headaches. In the latter case, testing may be done.


Diagnosis in Adults
If you are a young adult, most likely you will be tested for mono (Infectious Mononucleosis). If you are not a young adult though, your doctor may not even consider testing for EBV, unless your symptoms are very straightforward.
Doctors are just not looking for EBV in the older adult population because mono is assumed to hit young adults only. But mono is not what most adults are affected with. The concept of chronic activated EBV (CAEBV) as a chronic condition of recurrent EBV infections or even “chronic mononucleosis syndrome” is not something most medical doctors are aware of at this time, nor do they look for connections between CAEBV and autoimmune conditions, cancer, or many other medical complaints that have been implicated in EBV in research.
By the time you are in your 30s, 40s, or 50s, your chronic EBV may have reactivated a few times. In the meantime, you may have developed medical conditions as a result of CAEBV. This is, in fact, the population I work with most of the time. And this, I believe, is the most medically underserved group of patients. This is also where getting the right antibodies tested becomes a challenge.
Luckily, slowly, the medical map is changing. The very popular book Medical Medium by Anthony William has pried open the topic of EBV and its prevalence to millions of readers; now some are knocking on the door to their doctor’s office requesting EBV testing, suspecting that the medical complaints that have plagued their lives may be related to CAEBV. But since the medical community is still following a very narrow interpretation of blood lab results for EBV, there is a growing frustration in the patient population, and this leaves a gap that needs to be addressed: what to test and how to interpret the EBV labs, which is what I am just about to explain.
If You Need to Understand Your Test Results:
EBV Testing Results
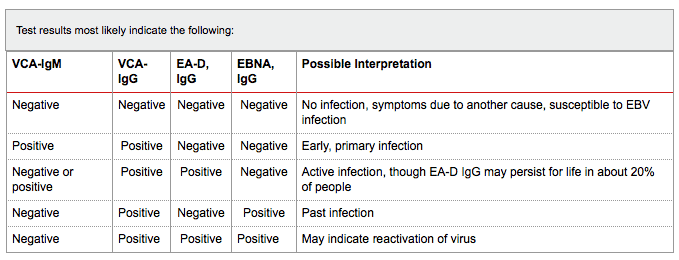
Here is the testing results table from Labs Online:
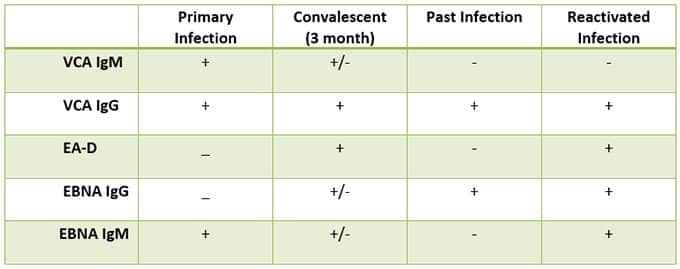
Here is another table, from Immunoscience Labs. Notice that it has an additional antibody, EBNA IgM. As far as I know, this is the only lab that tests this marker. I do appreciate it because I had a case when this is the only one that flared up, indicating ongoing infection. That would have been missed otherwise. This is rare to happen, but as you can see, it is possible.
Understanding the Big Picture
To understand the big picture and the cycle of the EBV “career” in your body, let’s look at some common scenarios, pitfalls, and important tips:
The presence of IgM antibodies indicates current infection or current reinfection; on a very rare occasion, we do see a person with a long-term positive VCA IgM, but that is unusual. IgG is the long-term and long-lasting antibody and may or may not be part of the current infection or reinfection.
EA-D IgG is the most important marker to look for to distinguish between past and current infection; EA-D IgG can mean that this is your initial infection OR that this is your current reinfection. This is the antibody that is most often left out of the EBV lab panel by doctors, so it is really important that you make sure your doctor does not skip it, whether this is your first or subsequent test.
Let’s say your VCA IgG is the only one that is positive (all four markers were tested). You cannot say definitively whether you have CAEBV—it depends on a few factors: have you had medical complications in your life, mono in the past, one or more autoimmune conditions, chronic fatigue, or perhaps cancer? In that case, is your antibody elevated only by a few points? Since this is the antibody that most of the population on the globe carries, positive VCA IgG alone does not mean much. It just means you have had exposure to EBV, and potentially, it can affect your health in the future. You may be perfectly healthy too. VCA IgG can stay positive all throughout your life. However, what if your VCA IgG is triple digits or “>600”? In that case, it is likely that you have chronic active EBV, but it is not reactivated at this time. Some people take very good care to maintain a healthy stress level, eat a balanced diet, get good restorative sleep, and live a healthy lifestyle in general, and they do not reactivate for decades.
Let’s say you had VCA IgG or other markers at “>600” and now you feel better but the numbers are still >600 at retest. This is often disappointing to people, but what you need to know is that many labs do not record the values higher than 600. What this means is that your initial values could have been at 5,000, and they may have dropped in half to 2,500 or even to 650 upon retesting. So even though the lab results still show above 600 (because your levels may still be above 600, and the lab doesn’t register the difference between numbers above 600), you may be improving. Do not get disappointed by the numbers—track your progress by your decreasing symptoms.
Let’s say your VCA IgG and EBNA IgG are positive, especially in triple digits, and your EA-D IgG has not been tested. The conclusion: you are not able to assess if you are currently in the reactivation or between reactivations. This is the most common error, and this is where many patients fall through the cracks, even for years, because they will be told they only had EBV in the past. Unless you test EA-D IgG, you cannot say for sure, so do not let that happen to you. Still, with both VCA IgG and EBNA IgG elevated, especially in triple digits, and with chronic conditions associated with CAEBV, you may still be suffering from CAEBV.
Let’s say that your VCA IgG and EBNA IgG are positive, in triple digits, and your EA-D IgG is negative. Especially with triple digits of the other antibodies, negative EA-D IgG means that you most likely have chronic EBV (CAEBV) but you are between reactivation. If you back track, you may realize, oh yes, during the holidays because of the different foods, family stress, travel, change in time zone, not enough sleep… you felt awful, sick, weak, etc. But when you did the test, it was four months later. Most likely, your reactivation happened around/right after the holidays, and by the time you got tested, the body had recovered from the infection.
Let’s say your VCA IgG, EBNA IgG, and EA-D IgG are all positive, and VCA IgM is negative. This means you are in the middle of your reactivation at this time.
Let’s say your EBNA IgG, EA-D IgG, and VCA IgM are positive. This means you are in the middle of your initial EBV infection (mono).
Let’s say your VCA IgG and EA-D IgG are high, but EBNA IgG is negative. The most important marker here is your EA-D IgG. You currently have infection/reinfection. Just like VCA IgG, 90% of population has the EBNA IgG antibody all their lives. However, 5-10% of the EBV population will fail to develop EBNA antibodies 5.
Let’s say most of your lab results are negative for VCA IgM. That is to be expected. This antibody only flares up during the initial EBV infection and it technically CAN show up during reactivation, but I really do not see that, and neither does Dr. Aristo Vojdani, who has tested a lot of people for EBV through his Immunoscience Lab. It is extremely rare to see VCA IgM positive with reactivation. With that in mind, if your VCA IgM is negative while other markers are high, of course you have a reactivated EBV infection at this time, and if VCA IgM AND EA-D IgG are both negative but EBNA IgG and VCA IgG are both high, especially in triple digits, you most likely have CAEBV but you are between reactivations (infections).
It is important to note that I have seen many irregular results that do not match these patterns, which is entirely possible as we are all unique. In fact, every antibody has its problems and complications, which I list more depth in my book.
What if all of your markers are negative, but you know you are sick?!
One answer is that your medical complaints may not be related to EBV.
However, we know that most people who carry EBV do not get sick, while those that do get sick often have a compromised immune system. To make sure your results are NOT false-negative, ask your doctor to do a simple blood test for total immunoglobulins: IgG and IgM (and I would suggest adding IgE while you are at it). If the total immunoglobulin IgG and IgM levels are low, you may need to recalculate your totals in the EBV test—it may have been negative because your immune system is so suppressed that it is not making enough IgM and IgG immunoglobulins, so you cannot trust the EBV test results to be negative!
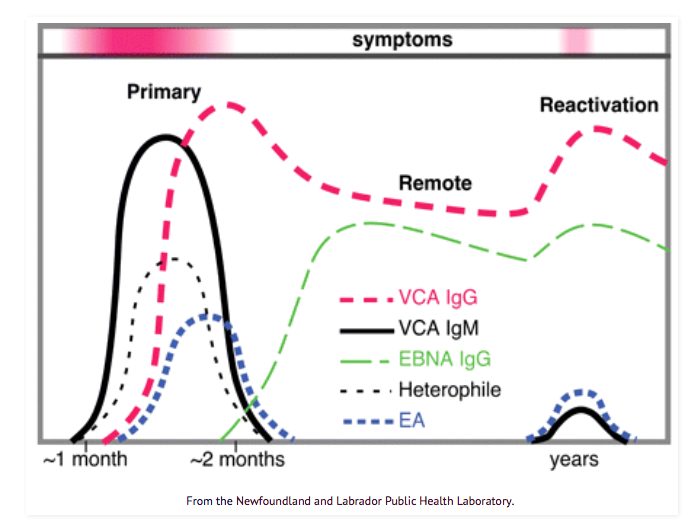
These were just the most important scenarios. Let’s take a look at a very simple graph—this is what helped me the most when I first began studying the interpretation of the testing.
I encourage you to look at this graph every time you get your lab results back.
As you see, VCA IgM is flared up in the very initial (primary) infection, within the third week I would say, and then it can show up again years after. But it is really rare or too low to be positive at recurrence.
On the other hand, VCA IgG starts showing after the first month or so of initial infection and then stays elevated for life. Again, this is the antibody most of the global population has elevated. This alone does not mean you have a chronic condition related to EBV. But as I mentioned, if it is very high, then it is a red flag, and you want to dig a little deeper.
EBNA IgG flares up only around/after the two first months of initial infection—this antibody also tends to stay elevated for the rest of your life. As I mentioned, positive EBNA IgG along with positive VCA IgG is not enough to suggest you have an active infection now unless you add EA-D IgG. You also have to consider your timeline, medical history, mono history, and symptoms. And this can simply mean that you are in between reactivations (this can last for years and decades).

What about PCR?
That is a very good question and a frequent source of misdiagnosis on the part of the medical community. PCR is basically DNA of EBV as found in blood serum of the patient; it is also referred to as viral load. Theoretically, this would be a great test to do on all EBV patients. However, studies are very consistent: PCR is ONLY a reflection of current EBV status if we are dealing with a current and most likely initial infection 1. This is what researchers have been finding. And when you think about it, it makes a lot of sense. EBV does not linger in your bloodstream. It soon leaves it for its preferred residence in your vagus nerve, central nervous system, thyroid, and other parts of the body, where it hides. It does NOT stay in your bloodstream to be found.
PCR is more sensitive than the antibodies we have discussed above and is 95% predictive of a primary infection, which is very unique, so if this is your first suspected infection and your immune system is low causing your antibodies to possibly be too low, then absolutely test it. But do it as soon as you can, so you do not miss it before it disappears; in most people, there is a rapid decline of EBV viral load within 2-25 days. So any time past 25 days, PCR may show negative even during the initial infection. I did find one study, however, which found 3% positive PCR in reactivated EBV cases 8, but that is rare.
PCR testing may be expensive, so check the price before you run it, and consider it more for a confirmation of an initial infection while you are in it, especially when your immune system is compromised and your immunoglobulins are not showing positive for EBV.
What about p22?
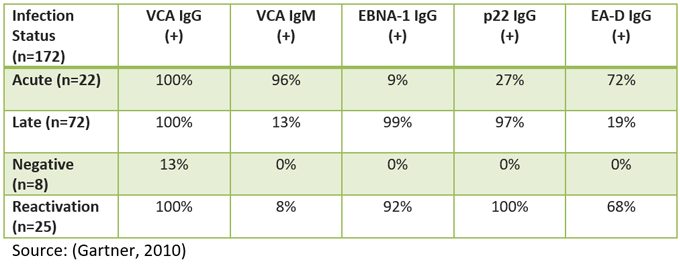
This is an interesting marker and may be very helpful, but it is not tested in the U.S. As you can see in the table below, in a German study, a group of 172 people with various stages of EBV (and one group without it) showed that all those with chronic EBV had positive p22 6.